
I struggle to keep up with Madeleine as she races down narrow, winding dirt paths through a maze of head-high corn stalks. She is a Community Health Worker helping to close the gap on access to lifesaving primary healthcare in remote regions of Togo, West Africa. In Madeleine’s hand is a mobile phone designed to make her lifesaving work more efficient. I pepper her with questions about the mobile application it houses and her experience using it. I am deeply curious about the benefits this technology provides, and whether they outweigh its costs and challenges.
This inquiry, which has me getting turned around and occasionally stumbling over rocks, focuses on the mobile health application recently launched by Integrate Health, in partnership with Medic Mobile. I am interested in learning if the tech we’ve been helping to co-develop for the past two years is benefiting the users who need it most, Community Health Workers and their patients. But I am also trying to situate our organization’s experience within the context of a burgeoning tech for global health field to better understand what is and is not working and most importantly, how we can do better.
I don’t claim to be an expert, but I do feel as though I’ve gleaned some insights from our organization’s own experience, over the past two years. I have also had dozens of conversations with technology companies, funders, other implementers and advisors. In the process of trying hard to get this right, I’ve learned three critical lessons that I believe could be relevant to others. First, tech is only as good as the system it aims to enhance. Second, good tech requires (a lot of) time, money, and really, really good people. Third, narrow solutions need to integrate.
Most importantly, I feel a deep obligation to talk honestly and openly about how difficult it is to effectively implement, not to mention scale, digital health solutions in extremely resource-limited settings. With new technology comes tremendous potential to drive health equity and help to deliver greater value for patients. But too often, tech solutions are being sold as a quick fix and an easy win. If we truly want to make progress, we must be realistic about the challenges before us. Fortunately, each of these challenges also represents an exciting opportunity, an opportunity that we cannot afford to miss if we want to leverage technology to advance health for all.
Tech is only as good as the system it aims to enhance
Madeleine loves her new android phone.
“It is much lighter than the old binder filled with forms I used to carry,” she explains.
Community Health Workers like Madeleine tote backpacks filled with basic medical supplies long distances over the hardscrabble terrain. Every pound that lightens the load makes the journey quicker and easier, which means covering more ground, visiting more homes, and seeing more patients in less time. That adds up to potentially more lives saved.
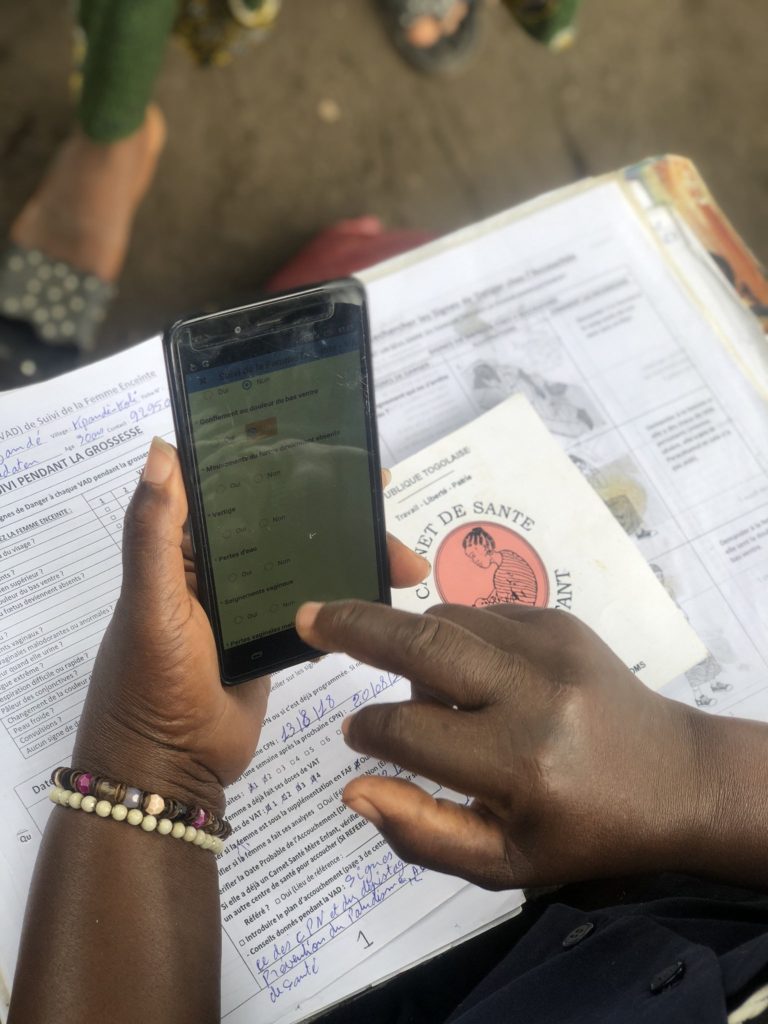
“When I open the application on my phone, it shows me exactly what I need to do that day,” Madeleine explains. “Yesterday I treated this child for malaria,” she points to a name on her phone screen. “This is my reminder to do a follow-up visit today. It also reminds me when to follow up with pregnant women.”
This is especially helpful as prenatal follow-up visits happen over a longer interval.
“I used to have to sit down each week and flip through all the pages of my notebook to see which women needed follow up. Now the application reminds me, a week, and again a day in advance. This makes it much easier for me to plan my visit schedule.”
This is a phenomenal example of technology amplifying the impact of a highly functional system. Community Health Workers like Madeleine receive training, sufficient supplies, dedicated supervision, and a salary to deliver professional healthcare services. This system was highly effective when it relied on paper-based supports and data collection tools. The introduction of a mobile phone and application, like that co-designed by Integrate Health and Medic Mobile, serves to enhance the efficiency of an already functional system. The application acts as a visit guide and provides decision support for Community Health Workers. It is lightweight, portable, and streamlines patient management. It electronically collects data to facilitate tracking, analysis, and subsequent quality improvement efforts.
But what happens when you layer technology onto an ineffective system? No matter how brilliant, a tech innovation is only as strong as the system it aims to enhance. This means that new technology can have only an incremental impact on solving the challenges caused by weak and ineffective health systems throughout the globe. Take self-diagnostic applications powered by artificial intelligence for example. Empowering a patient living in rural Togo with the capacity to diagnose a disease for which they can’t access treatment does little to improve the healthcare system or more importantly to improve health for that patient.
Don’t get me wrong, tech can be an important part of the solution, but it will never be the solution. Given that reality, it is important that the field of global health, including investors, funders, governments and implementing organizations be honest about the impact our dollars, time and energy can have when invested solely in tech. We must be sure that investments in health tech are additive and serve to enhance, not divert investments away from building and strengthening the underlying healthcare systems required to ensure that quality healthcare gets to the patients who need it.
Good tech requires (a lot of) time, money and really really good people
Kassan, a Community Health Worker in the rural community of Djamdé, echoes Madeleine’s experience. “The phone is much easier,” she assures me. “Why write lots of words when I can record the same information with just one click,” she says playfully. “My other nine fingers are growing lazy,” she adds laughing out loud at her own joke.
While the mobile application co-developed by Integrate Health and Medic Mobile has created time efficiencies for Community Health Workers, Integrate Health has had to make significant human resources investments on the backend. The number of staff, the technical skill level, the time and the financial resources required, have far surpassed our organization’s initial estimates.
At Integrate Health we collect a lot of data. And we use a lot of data. We believe deeply in the power of data-driven decision making and we’ve embedded feedback loops into all aspects of our program design to ensure that data is collected, reviewed, discussed, and used to drive continuous program improvement. Given the high volume and high level of interaction we have with the data we collect, our team had become well versed at diving into extensive excel spreadsheets. Now, with our data housed off-site with an external provider in an SQL database, we need both the in-house technical capacity and reliable Internet connection to access that same level of data. While we save time on data entry, we now require a full project management team with advanced technical competencies. Recruiting for this skill set in Togo has proved challenging. As our team grows to match the time, money, and human resources required to effectively implement the mHealth program, we are forced to reflect on how this program could eventually be managed by our partners in the Togolese Ministry of Health.
Across the continent, in Malawi, John O’Donoghue, now an eHealth specialist at University College Cork Ireland, described this very challenge. Referencing an application that proved useful in diagnosing children, he wrote, “even though the software was open source, the Ministry of Health just doesn’t have any internal capacity to roll out the software or even maintain it. Realistically if the project was to be modified and maintained and implemented we’re probably talking about a multimillion Euro effort per year”[1]. Another mHealth project that was scaled successfully by the Ministry of Health in Tanzania was attributed to “early recognition by the Ministry that the project would take at least five years of “burn-in” — meaning “understanding and absorbing and tweaking and optimizing”[2].
As Integrate Health has begun to explore both scaling our current mHealth application, as well as launching other tech projects, the one piece of consistent advice we have received is to find and hire amazing, talented people. One slightly larger organization we spoke with has seven in-house developers. Quant geeks, data architects, analytics scientists, and the significant financial resources required to find, hire and retain them, seem to be a prerequisite to effective implementation of technology projects in the new global health field. This is not necessarily a barrier to success. But it does raise the question of whether implementing organizations and Ministries of Health are prepared to meet these requirements. If a much greater level of human resource capacity is necessary to effectively implement and scale digital health programs, then organizations and Ministries, as well as those who fund and invest in them, must be ready to make the commitments necessary to enable these significant and essential human resource investments.
Narrow solutions need to integrate
This past summer, I was invited to attend a small meeting at the Gates Foundation. Much credit goes to the Innovative Technology Solutions team, which had convened a small group of implementing organizations and technology companies to explore how to build innovative tech solutions for Community Health Workers. Much to my surprise, the result of these discussions, stretching out over a couple days on their Seattle campus, was a consensus among the implementing organizations and the technology companies that what the field urgently needs are not in fact, more tools, but rather more incentives and support to integrate the tools that already exist.
Over the past two years, I’ve met with a number of different technology companies, each of whom has pitched me on an exciting product that I was eager to explore. In each of these conversations I was asked, “what do you really need?” Then told, “we only want to respond to your needs and help solve the challenges you are facing.” In each instance, I replied that I need what your product does, plus what these other three products do and I need them in one package. Usually, that request was met with silence.
Healthcare is not delivered in a single type of location or by a single type of provider. A child treated initially by a Community Health Worker, may later receive care at a clinic or hospital. Care moves with the patient. However, tech solutions, probably for some legitimate reasons, seemed to be designed for a specific delivery channel. There are Community Health Worker applications, Clinic applications, Stock management applications, Financial management applications, Health education applications, and Data aggregation tools. Even within one delivery channel, take a clinic, for example, different applications are required to collect patient data, manage stock systems and manage financial transactions.
Each of these applications or tools provides a solution for a part of the health system, but from where we sit as an organization working to strengthen an integrated primary healthcare delivery system, this fragmentation is deeply frustrating. Worse yet, these narrow solutions rarely, in our experience, integrate with one another.
While it is not impossible to imagine one tablet with multiple applications, it is absolutely essential that these applications talk to or at least share data with one another. In fact, the challenges posed by a lack of interoperability in the field of digital health are well documented[3]. But such integrations, albeit essential, are not sexy and therefore they are not well funded. Instead, the proliferation of contests, prizes, and pitch competitions focused on “innovation”, a buzzword synonymous with technology, has incentivized an explosion of new “things”. While mobile technology took an early lead in the prize-worthy space, AI, machine learning and all manner of seemingly silver-bullet tech-powered solutions have come to dominate. What has been lost in this over-hyped proliferation of new tools is the need for integration. As expressed by the group convened in Seattle, and others like OpenHIE (Health Information Exchange), this is the primary challenge. In my opinion, this also represents a tremendous opportunity. Integration is absolutely necessary if we have any hope of scaling effective technology solutions in resource poor settings.
A new path forward
I have no doubt that Madeleine and Kassan and the other dynamic female Community Health Workers, many of whom lack formal education, will quickly emerge at the forefront of the tech revolution in healthcare. What they need to accomplish this are not more innovations; but solutions that leverage effective systems, the funds to recruit and hire more skilled personnel and tech tools that actually work together.
They also need a community of leaders who are willing to step up and speak honestly about the challenges to scaling effective digital health solutions. We need to cut through the hype and focus on the real, important work that must be done collectively to move the field forward. Despite the challenges we face, I remain convinced that technology can play an important role in helping to drive more equitable and higher quality healthcare for patients. I am encouraged by the knowledge that there are already a lot of very smart people thinking about these obstacles. I hope that the solutions to these challenges are much closer than they seem.
Our ability to leverage technology to drive greater health equity will be determined not by our discovery of the next shiny thing, but by our capacity to make strategic investments in the systems necessary to ensure that these technological innovations actually work for patients. Investing in a database manager may not be as exciting as investing in a new phone app, but ask a Community Health Worker what she really needs and she will tell you, a bit of support will do. If we get these things right, strong systems, good people and integrated tools, we can unlock the potential and demonstrate the efficacy of community-based health systems led by women and powered by technology. If we get this right we can rapidly accelerate our path to achieving our ultimate goal, universal health coverage, health for all.
