Integrate Health is in the midst of an exciting process to restructure and strengthen our data management systems. The overarching goals of this process (as explained in our first post here) are to capture the full continuum of care, better align to the patient experience, and measure only what is useful for program improvement. In this spirit, Integrate Health recently revised our entire set of indicators, the measurement tools we use to know whether or not what we’re doing is working. While previously we had aligned to a traditional logic model, we now believe we have found a better way.
As a global health organization, we are well-versed in the use of logic models — the default tools used by international development organizations to demonstrate how organizations work. Per the CDC, a “logic model is a graphic depiction (road map) that presents the shared relationships among the resources, activities, outputs, outcomes, and impact for your program. It depicts the relationship between your program’s activities and its intended effects”.

Knowing that logic models can be useful, we had been using one to organize our activities and indicators around delivering high-quality primary care. We mapped out our primary goals — reducing under-five and maternal mortality — and then worked backwards to articulate the outcomes, outputs, and activities needed to achieve these goals. While this approach worked for a time, ultimately what we found was that this approach is not best-suited to an integrated intervention such as primary care delivery. Each time that we tried to apply the framework, we ended up creating program silos at the outcome level (e.g., reducing malaria morbidity, improving nutrition, increasing vaccination rates, etc.) and then having overlapping activities (e.g., improving Community Health Worker screening, improving medicines supplies, increasing effective referrals, etc.) that were necessary for achieving each outcome. Eventually, this led to diagrams that were just a spaghetti of lines connecting activities across health areas in a way that became completely indecipherable.
When we shared these preliminary drafts with our clinical staff, we received overwhelming feedback that models didn’t make sense because they weren’t consistent with how care is actually received by the patient and delivered by the health system. Healthcare isn’t delivered in a series of discrete, separate activities, but rather through a continuum of services, ideally fully integrated.
We needed a tool that could capture the measurement of these integrated activities more effectively.
Applying a framework that is consistent with care delivery.
Fortunately, our team had experience working with the Care Delivery Value Chain (CDVC) to map the delivery of pediatric HIV care in Togo and close delivery gaps. The CDVC describes all of the activities required to deliver care and illustrates their sequence and connections across all levels of the health system. By mapping a “patient journey,” the CDVC outlines the required activities at each stage of a patient’s interaction with the health system, revealing the relationships between activities and how they cascade from prevention to diagnosis, treatment, and the management of complications.
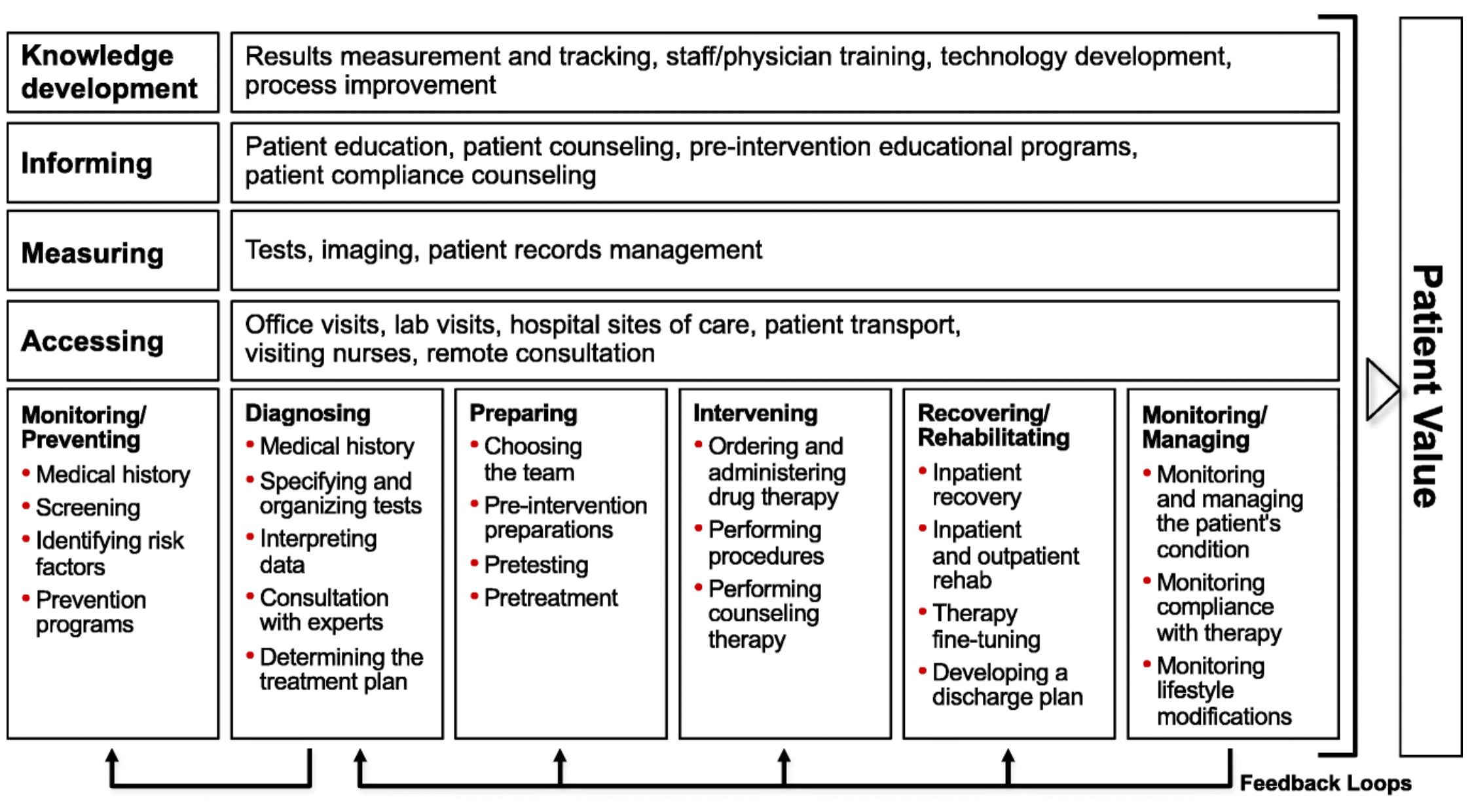
To apply the CDVC to primary care in Togo, we decided two value chains were necessary, corresponding to the two patient populations we serve — pregnant women and children under the age of five. Our teams then articulated the major steps required to provide care, preventative and acute, to patients in each population. For each step, the team listed the patient information needs, activities required, place where services are accessed, and measures to be collected at the patient level. Next, we added a row to track indicators that were relevant for each step in the CDVC. With a focus on the patient, the tool covered all of the major causes of death and all levels in the health system. Finally, we facilitated a participatory workshop that included program managers, clinicians, monitoring and evaluation experts, and partners in the Ministry of Health to review the framework and prioritize indicators. We received positive feedback as our participants generally found the tool to be useful, easy to understand, and a significant value add when thinking about programs.
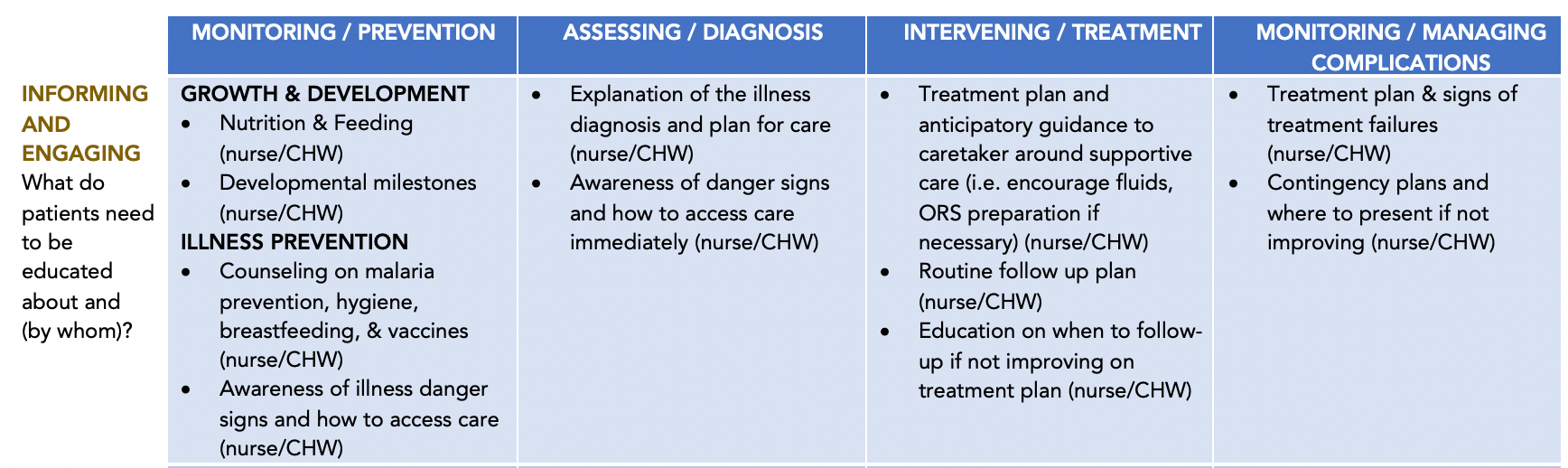
Overall, the CDVC proved to be a game-changer for our team. It helped build consensus on the activities and indicators needed to deliver high-quality primary care across the continuum of care for multiple conditions and across multiple levels in the health system. Consistent with Rhatigan et al, the framework provided a foundation for assessing primary care delivery for pregnant women and children under five. It helped to organize indicators in a way that was much more intuitive to our staff and partners.
Using the malaria example from my first post in this series, previously our only routine program indicator for tracking malaria was the number of children receiving malaria treatment within 24/48/72 hours. With the CDVC in place, we expanded indicators to cover the continuum of care including:
- the percent of children sleeping under a bednet (prevention),
- the percent of fever cases receiving a malaria test (diagnois),
- the percent of positive malaria cases receiving treatment (treatment),
- the percent of cases resulting in severe malaria (managing complications),
- and the number of deaths resulting from malaria (outcomes).
After participating in a workshop to build out the CDVC, our program managers began budgeting for funds to improve access to bed nets and to improve the transfer of patients from Community Health Workers to primary care facilities and secondary hospitals. Furthermore, for each step in the CDVC, our teams are looking across health areas including malaria and other neglected tropical diseases, neonatal disorders, HIV/AIDS, diarrheal diseases, and respiratory infections and identifying where activities could be coordinated to provide the best population health management possible. While this does increase complexity, the added context helps teams quickly pinpoint failures and align response activities accordingly.
Moving from silos to patient-centered care systems.
While logic models can be useful for demonstrating an organization’s strategy, they fall short when trying to measure how the primary care system will need to work to decrease mortality and morbidity.
A far better option is the Care Delivery Value Chain, and we recommend that all organizations working to deliver, or finance, primary care consider its use in program design and implementation.
The CDVC can facilitate communication around the integration of care across multiple levels and encourage teams to take responsibility for the full care continuum for a population or medical condition — encompassing prevention, diagnosis, treatment, and the management of complications. We call on donors and Ministries of Health to integrate care delivery systems, organize around distinct patient segments, and build the systems necessary to enable the transformation of healthcare in low-income countries from disease-specific silos to patient-centered systems. You can view our Pediatric Care CDVC here.
This post was written as part of a Data Series by Patrick Aylward, Chief Operating Officer at Integrate Health.
Biography
As Chief Operating Officer, Patrick Aylward is leading the transformation of Integrate Health’s systems to maximize the value of primary care delivery in line with Ministry of Health objectives. Patrick has over 15 years of experience working in global health in low- and middle-income countries with a focus on data-driven strategy and catalyzing markets for new products and innovations. Prior to Integrate Health, Patrick worked for Population Services International, Unitaid/WHO, the Global Fund, and Intel Corporation. He spearheaded the development of a global investment case for HIV self-testing; developed tools used to track medicine expenditure and patents in more than a hundred countries; and advised the Global Fund, the Bill and Melinda Gates Foundation, and other major donors on market dynamics strategies. He holds BA and MSE degrees from the University of Michigan and an MBA from Yale University.
